Plagiocephaly
As Millie got older, her parents became increasingly concerned as they watched the flat spot on her head get worse and worse. Her pediatrician suggested a helmet, but Millie also faced movement restrictions with her neck and jaw, and they knew the helmet would do nothing to help those challenges.

Mom and Dad tried to keep Millie off her back as much as possible, but thank goodness they listened to their gut instinct that kept telling them there was something more going on here, and there had to be a root cause of her plagiocephaly.
Unfortunately, for most parents, helmets tend to be the only option offered for plagiocephaly by traditional medical doctors and specialists. But this approach does not get to the root cause of the problem nor help with any mobility challenges, which Millie’s parents were rightfully concerned would affect her development as she got older.
WHAT IS PLAGIOCEPHALY?
Plagiocephaly is the flattening of a baby’s head on one side of the head or the whole back of the head. This develops when an infant’s soft skull becomes flattened in a specific area. It can get worse if a baby sleeps in the same position most of the time or because of mobility challenges with the neck muscles that result in a head-turning preference. Plagiocephaly is sometimes called “flat head syndrome.”
Plagiocephaly can often be mistaken for Craniosynostosis. Craniosynostosis is when a baby’s skull bones fuse together before they are supposed to. In Plagiocephaly, there is no fusion of the skull bones.
WHAT CAUSES PLAGIOCEPHALY?
Plagiocephaly is caused by repeated pressure on one part of the baby’s skull and is made worse when babies lie or sleep in the same position most of the time. This is a common occurrence in infants, and studies show that 20-25% of babies develop varying degrees of Plagiocephaly when they sleep on their backs.
Plagiocephaly can start to develop when babies are in the womb if they are stuck in an abnormal position and their head is tightly pressed against the uterus. This risk is higher with twins or multiples who have even less room in the womb.
Premature babies also have a higher risk because they spend significant time in the neonatal intensive care units (NICU) when recovering. They often lay in a fixed position for too long, causing plagiocephaly.
Muscular torticollis is a condition in an infant that causes a stiff, stuck, and twisted neck where the child’s head is continually bent to one side, making it difficult to turn and rotate their head and neck in both directions. Because of the neuromuscular tension and restricted movement caused by torticollis, it often causes or contributes to plagiocephaly in a big way, and many children struggle with both conditions simultaneously.
PLAGIOCEPHALY AND BIRTH TRAUMA
Birth intervention, such as the use of forceps or vacuum during delivery, has been associated with an increased incidence of head shape abnormalities, including plagiocephaly, in infants.
Several studies have investigated the relationship between birth intervention and the incidence of plagiocephaly. A systematic review and meta-analysis published in the Journal of Pediatric Rehabilitation Medicine in 2018 found that the use of forceps or vacuum during delivery was associated with a significantly increased risk of plagiocephaly.
Another study published in the Journal of Craniofacial Surgery in 2020 found that infants born via vacuum-assisted delivery had a higher incidence of plagiocephaly than infants born via spontaneous vaginal delivery or cesarean section. The study also found that infants who experienced longer periods of vacuum application had a higher incidence of plagiocephaly.
When you factor in how much physical strain and tension is placed on a baby’s head and neck during birth interventions, it’s perhaps most accurate to refer to it plainly as birth trauma. While the studies above mention forceps and vacuum extraction births, a rough c-section delivery can also lead to complications with plagiocephaly and torticollis for the child.
Plagiocephaly is perhaps one of the clearest and present examples of another lesser known condition called subluxation. Subluxation occurs when there is misalignment and abnormal motion within the neurospinal system, leading to an imbalance and dysfunction of the nervous system, known as dysautonomia.
Balanced and equal movement in the neurospinal system sets the stage for the skull to mold into a round shape all on its own. So when subluxation and stress on the nervous system interfere with that, it can lead to the development of plagiocephaly.
As Pediatric Chiropractors, our goal is to dig into the true root cause of a child’s presenting condition. While the more prominent component of plagiocephaly is the flattening of the head and facial asymmetry, the limited range of motion and subluxation is really the underlying issue.
WHAT ARE THE SYMPTOMS OF PLAGIOCEPHALY?
Symptoms of Plagiocephaly are pretty straightforward and can include the following:
- A visible flat spot on the side of the baby’s head or the whole backside
- The baby usually has less hair on the flat side of the head
- When looking down at the baby’s head, the ear on the flattened side may look pushed forward
- Imbalance of the ears, eyes, or other facial features
- In severe cases, the forehead might bulge on the opposite side of the flat head, along with other facial asymmetries
Plagiocephaly itself shouldn’t be painful for babies. The risk is that they will struggle to hit their developmental milestones due to the underlying issues with gross motor function, subluxation, torticollis, and so forth. This study shows that those delays will carry on into toddler years.
Additionally, kids with unresolved plagiocephaly will be more susceptible to ear infections and other respiratory infections since the subluxations and motion restrictions limit the body’s ability to drain fluid from the ears and move mucus through the respiratory and lymphatic systems.
TREATMENT FOR PLAGIOCEPHALY
Thankfully today, many parents do just as you are right now, exploring other options for plagiocephaly besides traditional medical recommendations of helmet therapy, physical therapy, and so forth. We strongly encourage you to keep looking beyond those options until you find the ones that truly do get the root cause.
Thankfully the treatment of plagiocephaly should never require medication or surgical intervention since the vast majority of cases do not involve a condition called craniosynostosis.
If your child went through any of the birth interventions discussed above, and you suspect your child may have subluxation contributing to their plagiocephaly and other challenges, the first thing to do is contact your local PX Doctor.
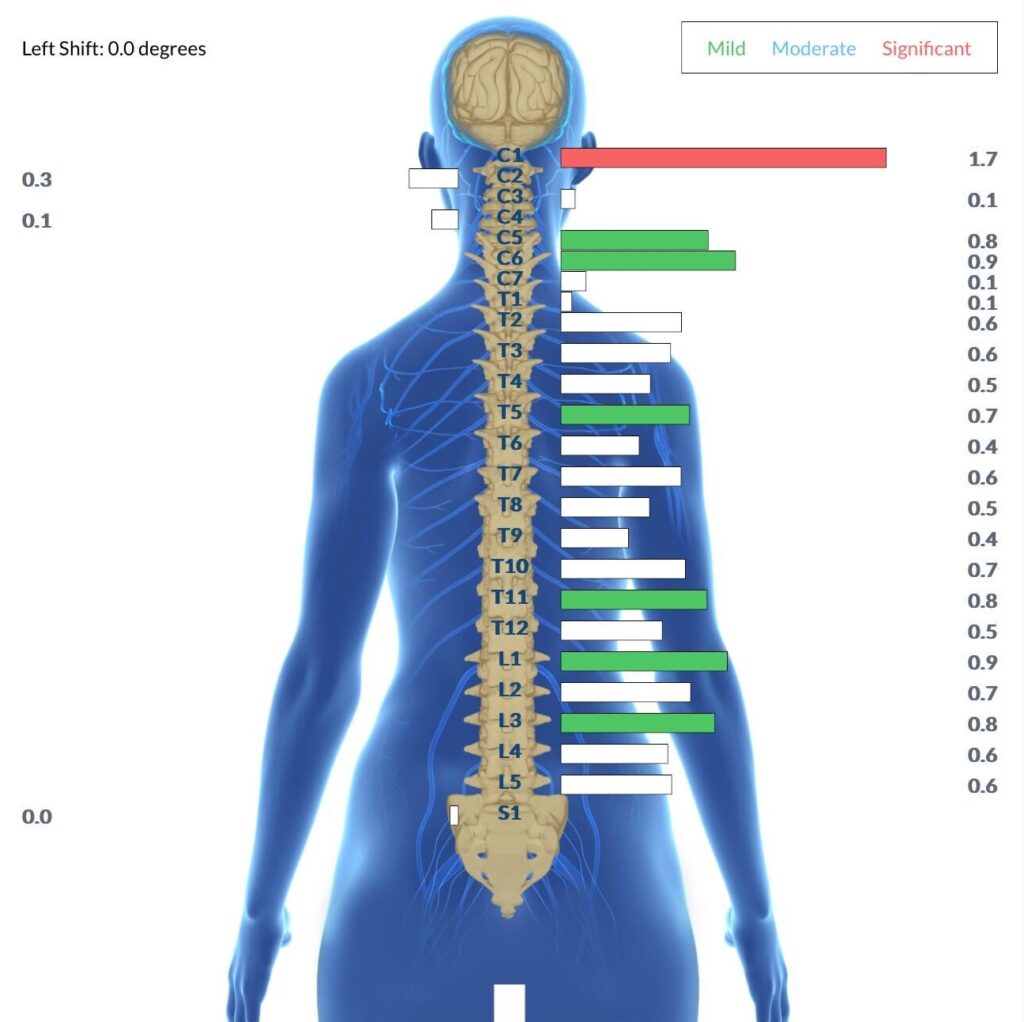
They will be able to find and locate the exact location and severity of the subluxation within your child’s nervous system using incredible technology called INSiGHT scans. These INSiGHT scans are safe, non-invasive, and reliable and take no longer than 15 minutes to complete.
Millie’s parents were not shocked when they saw on Millie’s neurological INSiGHT scans that clearly showed one side of her neck was more stressed and subluxated because of her limited movement. The significant subluxation shown by the red bar on the NeuroThermal Scan image below is the most common pattern our PX Docs see with plagiocephaly and torticollis cases.
Ensuring that plagiocephaly and any other underlying challenges are resolved in your child is crucial to their long-term health and neurodevelopment. Failing to address these issues could lead to the development of more complex challenges, such as gross motor delays, fine motor difficulties, sensory integration disorder, or even ADHD.
In addition to consistent chiropractic adjustments, we encourage ways to support your baby at home as well with the following home care options:
- Be sure to allow for plenty of tummy time and multiple positional changes
- Try to limit the time your baby spends in bouncers, swings, and car seats
- Alternate the side you hold your baby when feeding and carrying
FIND YOUR LOCAL PX DOC TODAY
Once your PX Doc has the INSiGHT Scans and exam done for your child, a customized care plan can be put into place. And then, from there, your PX Doc will make safe and gentle adjustments to relieve tension and address the subluxations.
Once Millie started chiropractic care, her parents began to notice improvements immediately. Millie shocked her pediatrician by only having to wear her helmet for a very short time.
The chiropractic adjustments were doing their job of getting her nervous system to a healthy place and clearing out those subluxations so her neck and jaw could move easily and her skull could continue to grow and mold properly.
Millie gained extra benefits, or positive “side effects,” of chiropractic care, including consistent bowel movements and overall happiness!
For more information on how Pediatric Chiropractor and our PX Docs Clinical Process works, check out the article and graphics here. And then, once you’re ready to get drug-free help for your child’s plagiocephaly, be sure to check out our directory and contact your local PX doc today!
ARTICLE SOURCES
Collett BR, Starr JR, Kartin D, et al. Development in toddlers with and without deformational plagiocephaly. Archives of Pediatrics & Adolescent Medicine. 2011;165(7):653–658. doi:10.1001/archpediatrics.2011.92
Collett BR, Wallace ER, Kartin D, Cunningham ML, Speltz ML. Neurodevelopmental implications of “deformational” plagiocephaly. Journal of Developmental and Behavioral Pediatrics. 2019;40(9):722-727. doi: 10.1097/DBP.0000000000000714
van Wijk RM, van Vlimmeren LA, Groothuis-Oudshoorn CG, et al. Helmet therapy in infants with positional skull deformation: randomized controlled trial. Pediatrics. 2014;134(3):e708-e715. doi: 10.1542/peds.2014-0405
van Vlimmeren LA, van der Graaf Y, Boere-Boonekamp MM, L’Hoir MP, Helders PJ, Engelbert RH. Effectiveness of positional therapy versus helmet therapy in infants with positional skull deformation (POSH): a randomised controlled trial. The Lancet. 2014;383(9920):1327-1332. doi: 10.1016/S0140-6736(13)62292-3
van Vlimmeren LA, Engelbert RH, Pelsma M, Groenewoud HM, Boere-Boonekamp MM, van der Graaf Y. The course of skull deformation from birth to 5 years of age: a prospective cohort study. European Journal of Pediatrics. 2016;175(9):1255-1262. doi: 10.1007/s00431-016-2763-6
Goh YH, Lim K, Chan YH, et al. Effectiveness of a baby pillow in preventing plagiocephaly: a randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2012;166(8):749–752. doi:10.1001/archpediatrics.2012.414
Speltz ML, Collett BR, Stott-Miller M, et al. Case-control study of neurodevelopment in deformational plagiocephaly. Pediatrics. 2010;125(3):e537-e542. doi: 10.1542/peds.2009-0052
Park MS, Lim SY, Han YS, et al. The relationship between birth-related factors and the severity of deformational plagiocephaly in early infancy. Annals of Rehabilitation Medicine. 2021;45(1):35-41. doi: 10.5535/arm.20453
Sun Z, Wu X, Xiang J, et al. Association between obstetric factors and head deformation in neonates. Pediatrics & Neonatology. 2019;60(6):647-652. doi: 10.1016/j.pedneo.2019.02.009

